If it shocks you to hear that clinical trials are getting more complex, you haven’t been paying attention. Specifically, we’re collecting more endpoints. We’re performing more procedures. We’re increasing nearly every executional variable, like the number of countries, the number of sites, the number of visits per patient, and the volume of data.
In fact, during our recent interview with Ken Getz of Tufts Center for the Study of Drug Development, he pointed out that over the past 20 years, they’ve seen this become a consistent trend.
But is the industry’s approach to clinical trial management making appropriate shifts? Making it through a clinical trial takes a lot of effort under normal circumstances. But today, with more data, sites, processes, and systems – it’s even more difficult.
Complexity in clinical trials isn’t bad
There are so many factors that contribute to the growing complexity of clinical trials. For example, we’ve seen a greater focus on rare disease therapies and more companion diagnostics. More precision medicine emerges each year, especially in oncology, which requires greater trial preparation as we outlined recently in our interview with Krystyna Kowalczyk of Oncobay. These kinds of treatments require researchers to collect more biomarker and genetic information at every step, even as early as screening.
Further, decentralized clinical trials and hybrid clinical trial protocol designs add complexities in execution as the industry adopts them at a more rapid pace.
And these complexities bring some great advantages. Some of the additional data leads to insights into new disease targets, or new applications for existing treatments. The adoption of more complex trial designs will bring clinical research to patients and communities previously inaccessible.
So, though more complex, these shifts mean progress, and hope for patients. Is complexity inevitable? Likely, yes – and so succeeding with clinical trial management in the future will require clinical operations leaders to accept that.
But trial protocol complexity degrades performance
Despite the benefits that this progress brings, Tufts research has found some drawbacks. In fact, clinical trial protocol complexity is inversely correlated with performance across all measures. Whether duration of the trial, from start-up to first patient in, and even closeout, performance decreases as complexity increases.
The more complex the protocol, the longer that cycle times are. More complex protocols also have far worse failure rates and dropout rates. Complex designs see much higher numbers of protocol deviations. They also experience a much higher relative number of protocol amendments.
The complexity will continue, so clinical operations leaders must find ways to adapt. More effective understanding of sites’ clinical trial readiness is a critical need in order to achieve a fast and smooth clinical trial start up. And better preparation leads to faster start up and is the best way to counteract the well-documented growth of clinical trial delays.
Effective clinical trial management in the future will require you to prioritize readiness of sites, teams, and caregivers
There was a time that leaders emphasized simplification of the clinical trial design. However, Getz acknowledged in our conversation with him that this was not the right goal. Reducing the number of procedures, or visits, or data endpoints is not realistic today.
Instead, he recommended a mitigation mindset. We have to find models of clinical trial management that promote success despite the growing complexities. This is especially true as we move into hybrid clinical trial models, where some patients will choose to participate remotely, and others in-person.
This is why we have to emphasize preparing and equipping people in a better way. Training the way we’ve always done it doesn’t fit a more complex future.
Data will be collected from new and complicated tools. It will come from various sources that have to be learned, installed, and integrated. Processes will involve patients that may be from remote regions, or caregivers that are in disparate timezones.
We must do better for our sites, caregivers, and patients. We can do that by adopting better training methods, and by better analyzing their real understanding of the content to identify where they need more support.
Clinical trial readiness as a benchmark
Using clinical trial readiness as the primary benchmark for selection of trial sites and team members also reduces delays, costs, and risks. An estimated 85% of clinical trials will experience delays, and site and staff readiness are major factors in delays. Clinical trial readiness is an overlooked, yet critical, way to increase the likelihood of a successful enrollment and ongoing study today.
Teams and sites that are better prepared are more likely to successfully recruit patients, provide better patient experiences, avoid protocol deviations, and meet deadlines.
From the sponsor’s perspective, clinical trial readiness mitigates risk in the face of complexity. Assessing and striving for clinical trial readiness enables project team leaders to better anticipate how their teams will perform.
Clinical operations leaders want to improve readiness
Before COVID-19 impacts hit, most life sciences organizations felt that they were effective in identifying site readiness and addressing issues. In fact, 76% said they were effective in identifying which sites were ready to start recruiting.
But the pause we took in 2020 likely put things into a new perspective. In our COVID-19 report, we discovered that 78% said they need to improve how they identify sites that are ready to perform.

A concept like clinical trial readiness, specifically trial site readiness, has been a disregarded but problematic reality for too long.
But understanding readiness will allow us to more efficiently spend time better preparing individuals to take part in complex clinical trials.
What clinical trial readiness means in practice
What is clinical trial readiness? We write about this topic in great detail, but in summary: readiness is a measure of how prepared an individual, team, or site is to perform during a trial.
Readiness can be measured in a number of ways, like:
- Level of comfort with key study outcomes.
- Ability to make good decisions in patient eligibility.
- Confidence with SOPs and systems.
As the protocol, and the processes, become more complex and nuanced, those performing a clinical trial need more and better support. We must find ways to prepare them for the challenges ahead, especially new ones.
For more details, you can grab our comprehensive guide to clinical trial readiness.
Here is a very real example. In our podcast, Getz shared that Tufts has been doing more research into patient dose non-adherence. The group estimates that about half of all patients will intentionally not take at least one dose.
How are you preparing your sites or caregivers to deal with this? You can – and should – address it directly.
- Train site staff and caregivers on patient non-adherence.
- Assess their ability to work with patients to prevent non-adherence, and proper intervention and follow-up.
- Analyze who needs more support, and who is best equipped to address the issue.
- Gather feedback and insights around how to better help sites, caregivers, and even the patients themselves to adhere to the dosage.
- Distribute best practices from the site staff and caregivers who have proven to be ready.
Clinical trial management solutions can help you now
The clinical trial is a complex set of processes, with many steps and people involved. The more complex the protocol, as well – the more risk there is to the timeline.
And if you don’t meet study timelines in the trial start-up, it greatly impacts the likelihood of missing other study milestones in the future. This is why it’s so important to prioritize the success of our sites and participants. Knowing who needs help – and in what area – will move everyone ahead faster.
Don’t look at growing complexity as a problem, but instead as an opportunity to drive overdue improvements. It is a reason to establish new and better processes to pave a path for running better trials. An opportunity to better support the site staff who will be caring for patients as they test your therapy. A step towards reducing your risk and error. And for embracing a future where you may run a truly decentralized clinical trial, or even a fully virtual trial.
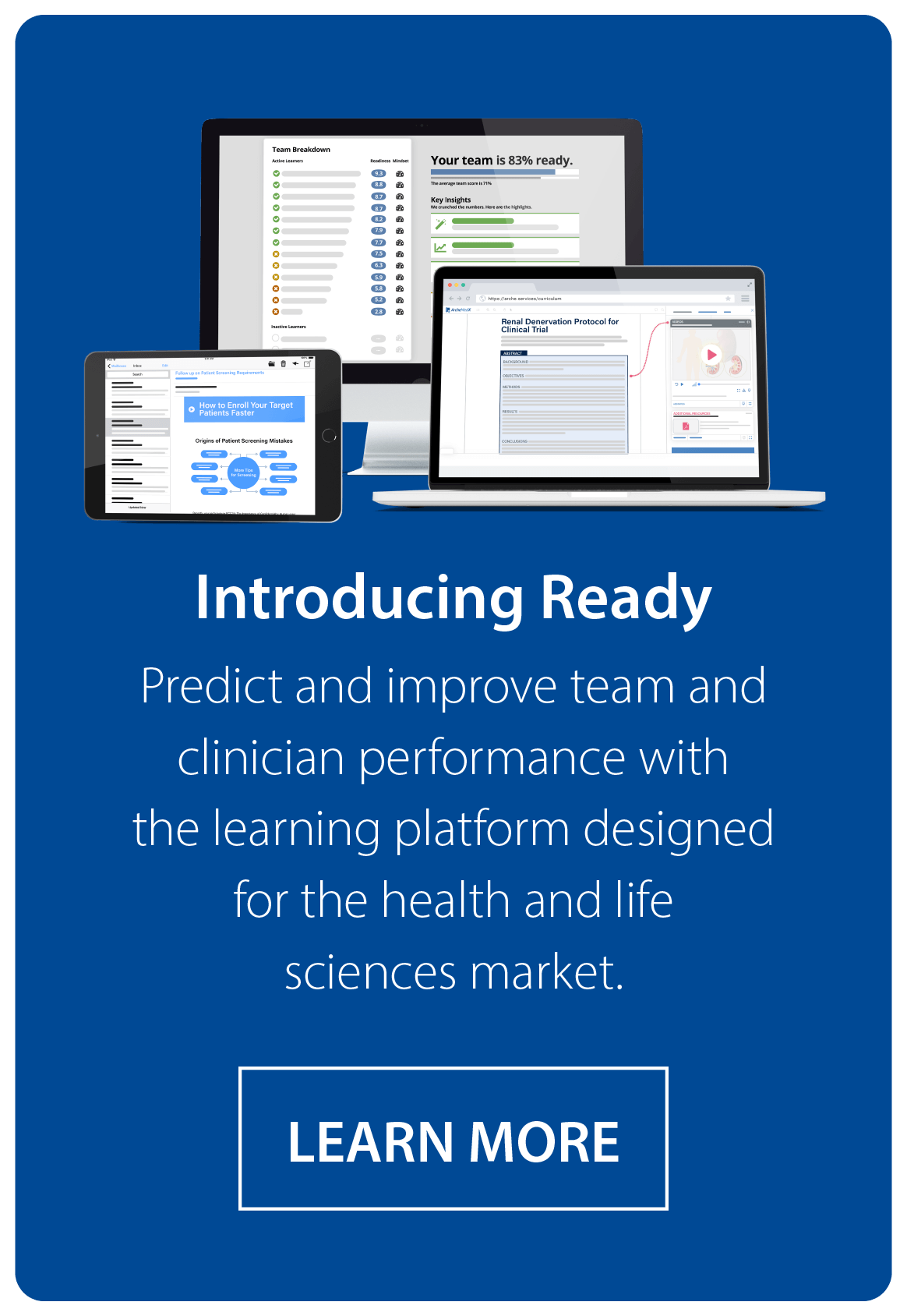
Technology will make this shift much easier, and it can also deliver benefits to the rest of your team if you recognize these three challenges, and plan for them. Ready by ArcheMedX can help you improve your clinical trial start up, while you improve your site and team performance (and ease their workload, too).
Successful clinical trial management as complexity grows is going to require a focus on better preparing everyone in your trial. The first thing you need is an approach, and clinical trial readiness is an ideal one. Learn more in the Definitive Guide to Clinical Trial Readiness.