The decentralized clinical trial is one of the most talked-about emerging trends in the life sciences industry. These sorts of clinical trials present immense benefits, as we wrote about in a recent blog.
If executed well, the decentralized clinical trial design could both reduce resource consumption and accelerate treatments arrival to the patients that need them.
But to realize the benefits of a decentralized trial, it’s important to understand that decentralization means education at scale. It means training at scale. Because obstacles like patient treatment adherence, consistency of performance, and data collection loom large, it means you have to find a way to educate and train, assess, and then probably re-train in a way that doesn’t stretch your resources.
And it’s realistic today – if you can implement a few key changes.
Decentralization means a focus on results, not just training.
In the traditional clinical trial design, you have the ability to look at very discrete activities that can be tracked and completed. Each investigator or site can become a milestone on the big-picture plan.
But in a decentralized clinical trial, you lose some of the core group dynamics that come from the reliance on centralized study locations. You could be working with people in faraway regions who are much less experienced than you in clinical research. Or you may encounter healthcare practitioners with only a single patient. Or – you may be engaging with mobile nursing or care teams.
Traditional clinical trial site training was created for a scenario where people are face to face with an instructor, and perhaps have one another to lean on afterwards.
As we decentralize clinical operations, we have to shift away from the idea of “completing the training task” and shift into the concept of “driving results.”
And in case “results” feels too obtuse, let’s get specific. Start thinking about how you equip your trial team to:
- Meet your overall enrollment targets. Where a centralized clinical trial site may have had specific site targets, a decentralized trial design doesn’t mean that.
- Avoid deviations. Decentralization opens the opportunity to participate in a clinical trial to many more patients (and their caregivers) who may not have a lot of exposure to the process.
- Deliver the data and results effectively. There are going to be questions, and lots of retraining. If you accept that, and plan to make and maintain clinical trial readiness as a goal for your trial team members, you will reduce the effort on your part – and on caregivers’ parts.
A decentralized clinical trial demands quality control. Don’t make that more work – it should be less.
Excited to spend days turning your protocol document into a 200 site initiation presentation? No?
Good, because that’s wasted time. When thinking about a decentralized clinical trial, you need to ensure quality and consistency. Your goal should be to see how much you can reuse to reduce your workload.
Focus on the content you’ve already gotten approved. Then spend a fraction of that time you were planning to invest in converting that slide deck into a far more useful exercise. Instead, use a platform like Ready to create learning moments and resources that focus each learner’s attention on the key points that need emphasis.
You’ve saved dozens of hours on slide creation, so use it to build content that emphasizes critical protocol points.
Protocols are rarely optimized for use by trial site staff, doctors, or personnel. This can become even more critical in a decentralized clinical trial. So think critically about where a set of new eyes might miss a point.
Where could a caregiver need more detail or more scientific background? At what points could you add some additional materials to better support the protocol? Where are trial staff making notes, asking questions, or providing key pieces of implementation feedback?
Some things we’ve seen work well in other clinical trials:
Videos presented by research or development team.
Video is also extremely powerful for keeping someone engaged. Today, you can quickly produce a video using a variety of tools. For example, your medical director could record a 90 second talk using their iPhone on the importance of the study. Or use a personal Zoom meeting to combine a site training powerpoint, with voiceover, or even music to break up the viewing experience.
Infographics and visual ways to present past phase results.
Charts, graphs, flowcharts, and simple images are all effective to engage people visually with concepts you’ve included already in written copy, and they can all be created by anyone with a computer and the Internet.
The great thing about engaging people is that they’re more likely to retain the information you’re putting in front of them. A video or well-designed image will engrain a point into the staff member’s memory.
Embedded quizzes or prompts to nudge participants at key points in the protocol.
It’s a common best practice to use real world scenarios or vignettes to drive critical thinking during learning activities. This also helps break up the learning experience.
If you’ve delivered a case study in a large group at an investigator meeting, you can easily transition that to digital exercise. Virtually, individuals must complete the activity, rather than sit as you walk through the entire story with limited interaction. Completing the activity themselves helps to attach meaning to the content you’ve provided them. That meaning is what prompts the recall of the concept in the field.
Make your vignettes complex, and make them as realistic as possible. And make them take a decision while thinking critically. Remember that you are equipping people that will have to deal with real patients and real risks during a clinical trial, and they may be without experienced clinical staff that would exist in a larger study center.
Distributed clinical teams need ongoing training and support. Plan for that.
We’ve mentioned the Forgetting Curve in previous posts. It’s well-documented that humans will forget 70% of what they learned in 24 hours. We retain information better when it’s repeated.
So it’s important to build a cadence of communication to re-emphasize points that need to be retained or remembered. But a cadence like this can help you in other ways.
There’s a trend of CRAs or trial managers sending out “newsletters” hoping to deliver best practices or updates. These can quickly become noise – and worse, vary in quality and accuracy.
In a decentralized clinical trial, there are many more people to remind, engage, and update. Establish a schedule, and centralize the execution for your dispersed personnel.
Our clients tell us that they use Ready to develop regular, ongoing communication streams with our Boosts feature. During a trial, these clients use the automated Boosts to deliver best practices that they discover from caregivers, updates to processes, and even amendments to the protocol.
Embrace technologies that support asynchronous delivery and decentralized teams.
In losing the centralized study training models, you also avoid the struggles of coordinating calendars and travel with very busy people. Embrace the flexibility of asynchronous learning, that is – delivering your clinical trial content on-demand.
Decentralized teams may span geographies and time zones, and you could easily spend days or weeks trying to deliver various sessions to accommodate all. Instead, choose technology that lets you deploy once, and update centrally.
Asynchronous learning isn’t the same as a recorded video, that can fail to engage or deliver any measurable results. In fact, the opposite can be true.
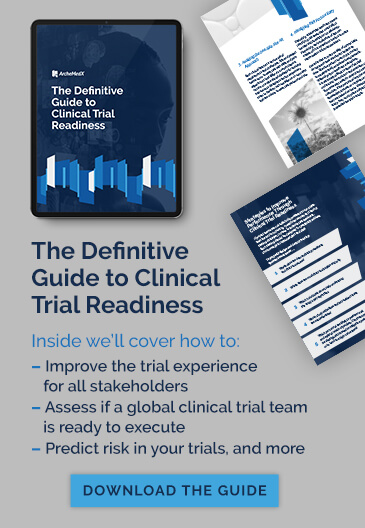
We blog frequently about clinical trial readiness, and a large part of readiness is the ability to measure. That is, understanding how capable and confident personnel are with applying your content.
As we described previously, metrics are both available and important for clinical trial readiness, especially in a remote clinical trial.
For example, imagine your entire clinical trial team completes an online presentation covering your upcoming trial protocol. Do you present them with a quiz to test their recall of critical information?
If you do, some of the team might answer correctly because they have gained the knowledge and are ready to apply what they have learned in your trial. Others, however, may get through the test by guessing. Perhaps they all pass.
If they do, are they all equally prepared to conduct your study or are you releasing under-prepared staff, patients, and caregivers into the field alongside others who are ready to make good decisions. Without measuring readiness, which is what we drive towards with Ready, you won’t know how risky this is until you run into trial delays and deviations, or worse.
Ready by ArcheMedX makes decentralized clinical trial training scalable.
There are still a lot of challenges for life science companies that want to deliver a decentralized clinical trial. Fortunately, there are some strategies that will deliver benefits to any clinical trial – and developing a scalable approach to educating clinical trial teams is one major opportunity.
The first thing you need is an approach, and clinical trial readiness is an ideal one. Learn more in the Definitive Guide to Clinical Trial Readiness.
Second, you need an on-demand delivery platform for learning at scale, and Ready by ArcheMedX is the only learning and insights platform designed to better equip clinical trial teams. Ready is an ideal tool as you work to adopt the decentralized clinical trial design, and you can get a demo today.