When a Sponsor chooses to engage with a contract research organization (CRO), the Sponsor team expects quality and performance in return for their investment. CROs are in business to conduct trials – and offload the work from the Sponsor’s side. So why are so many trials fraught with early hiccups? The truth is that there’s limited clarity – and agreement – around what it means to be fit to start, or clinical trial readiness. Most Sponsors have no process for that readiness – and unfortunately, neither do most CROs.
We recently conducted a survey which revealed that 78% of clinical operations leaders say they need to improve how they identify sites that are ready to conduct a clinical trial.
More effective understanding of sites’ clinical trial readiness is a critical need in order to achieve a fast and smooth clinical trial start up. And a fast start up is the best way to counteract the well-documented growth of clinical trial delays.
Thus, creating a center of excellence around clinical trial readiness is a huge opportunity for CROs to carve out a differentiator and value proposition.
So how can a CRO best help sponsors with clinical trial readiness? There are four main ways:
- Lead Sponsors to a better understanding of what clinical trial readiness means.
- Simplify how you measure and remediate site readiness.
- Provide your Sponsors full visibility into site (and trial team) readiness.
- Use your clinical trial readiness measurement process to uncover and address risk areas.
Lead Sponsors to a better understanding of what clinical trial readiness means.
What does it really mean to be ready?
It’s imperative that a CRO partner help Sponsor clients to answer this question. A leading CRO should help the Sponsor understand that clinical trial readiness can be defined, and measured.
First, clarify that readiness is a measure of how prepared an individual, team, or site is to perform. Then, identify what that measure should include, such as:
- Level of comfort with key study outcomes.
- Ability to make good decisions in patient eligibility.
- Confidence with SOPs and systems.
In the past, most trials have had little rigor around site selection, using various dubious methods. That doesn’t have to be the case, because if a CRO and Sponsor can establish expectations, they can measure individuals against those expectations.
For more details, you can grab our comprehensive guide to clinical trial readiness.
Simplify how you measure and remediate clinical trial readiness.
Before COVID-19 impacts hit, most life sciences organizations felt that they were effective in identifying site readiness and addressing issues.
In fact, the survey I mentioned earlier revealed that 76% felt they were effective in identifying which sites were ready to start recruiting. But when probed more deeply, that confidence fell.
Markedly fewer, at 56%, felt confident they could effectively measure site understanding of inclusion and exclusion criteria.
Fewer still, at only 51%, felt confident they could measure which sites understood investigational product and sample management pre-COVID.
Now, the pandemic has changed perceptions dramatically. Now that in-person visits and meetings are greatly reduced, trial teams can’t make decisions on gut feeling.
So now is the perfect time for CROs to establish capabilities around measurement of sites’ capabilities and readiness to start. To do so, a CRO should craft a plan for what metrics can be assessed for site staff and trial team members. One of our recent blogs covered some of these clinical trial readiness metrics for site selection.
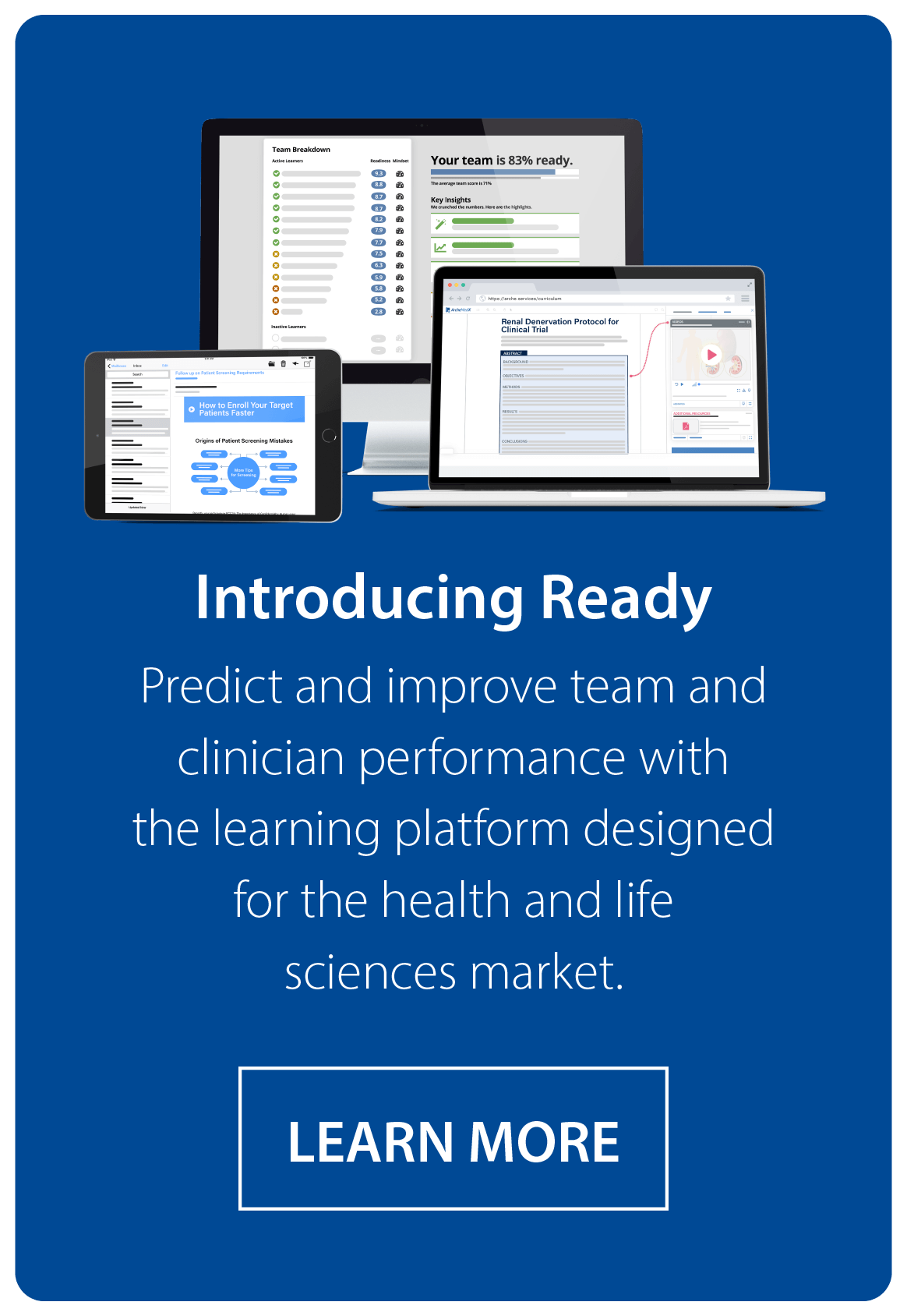
CROs who use Ready are able to tap into these metrics to create a consistent readiness score for individuals, sites, and teams. Using these metrics, or the readiness score from Ready allows a CRO to:
- Prioritize sites for early and subsequent start based on likelihood of performance.
- Simplify the transition from subjective to objective site selection for a Sponsor.
- Greatly reduce the work involved in site selection by automating it.
- Identify specific areas for remediation by individual and site.
This final point is important – because though a site may not be ready to start right away, some individuals and sites will only need a little additional help to become ready. Using more rigor to assess individuals like we do with Ready makes it crystal clear who needs what help.
Provide full visibility into clinical trial readiness
One powerful way to help Sponsors is to provide real-time visibility into the status of the trial, and that begins with site readiness.
Imagine reducing the questions from a Sponsor’s team because they can view information in real-time. Imagine exposing the level of confidence and capability for critical staff like the current study coordinator, the principal investigator and sub investigators.
You may wonder how this is done. Once you’ve determined an approach to measurement (by choosing what to measure, and what metrics to use), a CRO must find a way to measure those metrics.
There is so much opportunity for data sharing available with digital clinical trial solutions today. If you are using technology to assess your sites, you can expose that progress data to your Sponsors.
CROs that do this deploy a remote interactive experience to prospective sites using a tool like Ready. Using the clinical trial protocol synopsis and key questions, CROs observe the site personnel engage with the content.
In real time, the Sponsors and CROs measure their readiness and fit automatically. As a bonus, these Sponsors and CROs also gather key inputs about the viability of the protocol first-hand.
CROs and Sponsors can quickly uncover the site personnel strengths and weaknesses. Further, they can see engagement levels, and how sites rank vs. other potential sites. This directly enables a CRO to decide the order in which they should initiate sites to drive the best and highest quality enrollment.
Armed with this data, those trial teams know exactly which sites are most likely to succeed with the trial’s requirements. Even more exciting, they have new visibility into the risk areas for ill-prepared sites, and can stop guessing about site problems.
Identify site and individual risk areas early.
Shockingly, more than 1 in 3 clinical operations professionals struggle to know where and how best to help trial sites that aren’t ready to perform a trial.
Most site problems fall into three categories:
- Recruitment
- Data and documentation
- Protocol adherence
You probably have many SOPs and processes around addressing each of these. But most CROs wait to address the problems until after they appear – instead of trying to prevent problems.
Some might suggest that additional clinical trial team training will reduce the downstream delays. That could be true but why put every site and staff member through additional training? Wouldn’t it be better, faster, and possibly cheaper to identify risk areas before you start with a clinical trial site?
The best way to prevent clinical trial delays is to find potential risks before they erupt.
Measuring clinical trial readiness by site allows you to start your trial with sites that are less likely to experience problems.
For any site risks you identify that you can address, you will be able to revert to the remediation plan you established. Now, you can invest time and resources to upskill all or just some of those sites. Simultaneously, you can begin with limited delays from the best-equipped sites.
How does this work?
As I described above, using a clinical trial solution like Ready, which is focused on not just training your clinical trial sites, but on predicting their performance, allows you to spot the high performing sites and those with gaps in knowledge or capability.
When you know where the risks are, you can address just those areas. Reduce the work that you put in – and that sites put in. And invest only in those sites that are high opportunities to achieve readiness.
Sponsors want to improve clinical trial readiness. If CROs make it a focus, they can scale that knowledge across their various Sponsors.
The entire industry has always struggled with effective site training and needs better approaches — regardless of the pandemic.
According to Tufts CSDD, nearly half of all sites under-enroll or fail to enroll a single patient, forcing clinical trials to increase the planned enrollment period by 94% to meet targets (Source: Tufts CSDD, 2017).
There is huge room for improvement. And we can solve this problem if we can be more prescriptive in identifying which sites are truly well-equipped and ready to enroll patients.
Sponsors have clearly indicated that better clinical trial readiness is a priority for them. And if CROs take the lead on improving their approach to this, they can scale the improvements across the industry faster.