Getting new treatments approved has never been harder, but recent research reveals that the regulatory agency has also never been faster. So why is it getting more expensive and taking ever longer to bring a treatment to market? Three words: Clinical trial delays.
It’s taking longer to bring a treatment to market, and clinical trial delays are partly to blame.
A recent study by Tufts Center for the Study of Drug Development revealed some shocking news: the clinical development of new drugs is lengthening, and not by days, but by months. This, despite regulatory approval time for new drugs in the United States shortening.
The actual numbers?
Average clinical phase time increased by nearly seven months. Approval times dropped during the same time by nearly two months. In total, the time to conduct clinical studies and then complete the approval phase increased by 4.8 months.
This is a worrisome trend, worsened by our current environment fraught with delays due to COVID-19. So why is it happening?
Like any question in clinical research, the answer is complicated. However, we can point to a few truths:
- Despite approval times reducing, regulatory agencies are keen for sponsors to include longer follow-up phases.
- The treatments and associated trial designs continue to become more complex.
- Delays continue to plague all phases of clinical trials.
Only the clinical trial delays are within your control as a sponsor or contract research organization (CRO). It’s well-documented that 85% of trials will experience a delay, so reducing delays is a worthy undertaking.
Let’s take a look at three places where you can – and should – stop guessing: investigator meetings, clinical trial site initiation, and clinical trial site problems.
1. Stop guessing about your investigator meetings.
When planning an investigator meeting agenda, many make assumptions about what the investigators know, and what they don’t know. We guess about what content they will find challenging and what they will find easy. And we guess about where they are going to need help. We guess…quite a bit.
Why? There are so many ways to surface what the attendees actually already understand today. We can use digital survey tools, through pre-assessments, or online knowledge analysis.
There’s no reason to play this guessing game today and waste valuable time during the meeting. That wasted time could be spent emphasizing the critical topics that the investigators and study coordinators really need to know better.
Better-prepared investigators and study coordinators will beget better-prepared clinical trial sites. Those sites will be better able to enroll and conduct your clinical trial, with fewer delays.
So how can we stop guessing? Some sponsors distribute a survey or ask for feedback after sharing a protocol synopsis. Others use a clinical trial solution like Ready to deliver a pre-meeting assessment or pre-meeting content. Doing so helps to understand attendees’ initial knowledge of and comfort with the planned study.
Investigator meeting content delivery will engage PIs and Study Coordinators around the content and critical questions ahead of time. This provides valuable insight to meeting planners and content developers.
Want to go further? We recently covered how to deliver a fully virtual investigator meeting. A virtual investigator meeting will enable you to create a learning track that takes the same amount of time to develop, and much less cost to deliver. That’s because you can:
- Prioritize content and topics based on pre-tests
- Deliver the entire investigator meeting remotely and on-demand (reducing travel and meeting planning costs, and preventing delays at sites where the PI can not travel)
- Prioritize follow-up content based on how the investigators and site staff perform in the training
- Automatically send follow up content to re-emphasize critical points
Taking the guesswork out of creating your investigator meeting content, virtual or not, is a proactive step you can take to ensure that investigators and coordinators are prepared to operate at their highest level of performance.
However, doing that alone is not going to eliminate clinical trial delays. Making your clinical trial site initiation process more accurate might.
2. Stop guessing in your clinical trial site initiation.
Many sponsors and CROs make decisions about which sites to initiate and when to initiate them using primary tools that are a bit outdated. Examples include: attendance records for investigators invited to the PI meeting, outdated historical site data, and site-provided data which could have dubious origins.
Sometimes, sites guess or inflate the number of patients that they believe they can enroll when completing the traditional site feasibility assessment. Sponsors and CROs anticipate this response and typically adjust the projections to fit their expectations for each site.
So sites are guessing, and sponsors and CROs are responding to that with more guessing. And for an industry so focused on data endpoints and statistically relevant evidence, it’s shocking. This makes the frequency of delays in these clinical trials much more understandable.
If you knew that removing the guesswork would reduce your clinical trial delays, wouldn’t you find a way to do so?
More accuracy in clinical trial site initiation will reduce delays. And it is possible to achieve.
There is so much more accuracy available with digital clinical trial solutions today. As Kelly Ritch wrote previously: “We can leverage proven digital technologies and behavioral analysis to evaluate site feasibility in a more novel way that assesses the confidence, capability, and interest of site personnel.”
We can leverage proven digital technologies and behavioral analysis to evaluate site feasibility in a more novel way that assesses the confidence, capability, and interest of site personnel.
For example, combine your historical site data and performance with current, and specific, context to find the right-fit sites to initiate for any particular study. Measures can include the level of confidence and capability in this particular study’s area of focus for critical staff like the current study coordinator, the principal investigator and sub investigators.
Or you could analyze these sites’ commitment to recruiting subjects for your study vs. their existing studies.
You don’t have to restrict yourself to data that the site provides. Using a clinical trial solution like Ready, you could be delivering not only a remote investigator meeting, but a fully remote site analysis. Then you could determine which sites have both the historical performance and the current aptitude to succeed.
CROs and sponsors who do this deploy a remote interactive experience to prospective sites using the clinical trial protocol synopsis and key questions. As the site personnel engage with the content, the sponsors and CROs can measure their readiness and fit automatically. As a bonus, these sponsors and CROs are also gathering key inputs about the viability of the protocol first-hand.
The CROs and sponsors can quickly discover the site personnel strengths and weaknesses, their engagement levels, and how they rank vs. other potential sites. This directly enables them to decide the order in which they should initiate sites to drive the best and highest quality enrollment.
Armed with this data, those trial teams know exactly which sites are most likely to succeed with the trial’s requirements. Even more exciting, they have new visibility into the risk areas for ill-prepared sites, and can stop guessing about site problems.
3. Stop guessing about the clinical trial site problems.
More than 1 in 3 clinical operations professionals struggle to know where and how best to help trial sites that aren’t ready to perform a trial.
Most site problems fall into three categories:
- Recruitment
- Data and documentation
- Protocol adherence
You probably have many SOPs and processes around addressing each of these. But why are you waiting to address them as they appear?
Some might suggest “additional clinical trial team training will reduce the downstream delays.” That may be true, but wouldn’t it be better, faster, and possibly cheaper to identify risk areas before you start with a clinical trial site? You may not have to push every site or staff member through additional training.
The best way to prevent clinical trial delays is to stop waiting, and be proactive. If you revert back to tip #2 – you reduce two different ways:
- By starting your trial with sites that are less likely to experience problems
- By identifying and remediating risk-prone sites before you start with them
Now, you can invest time and resources to upskill all or just some of those sites. Simultaneously, you can begin with limited delays from the best-equipped sites.
How does this work?
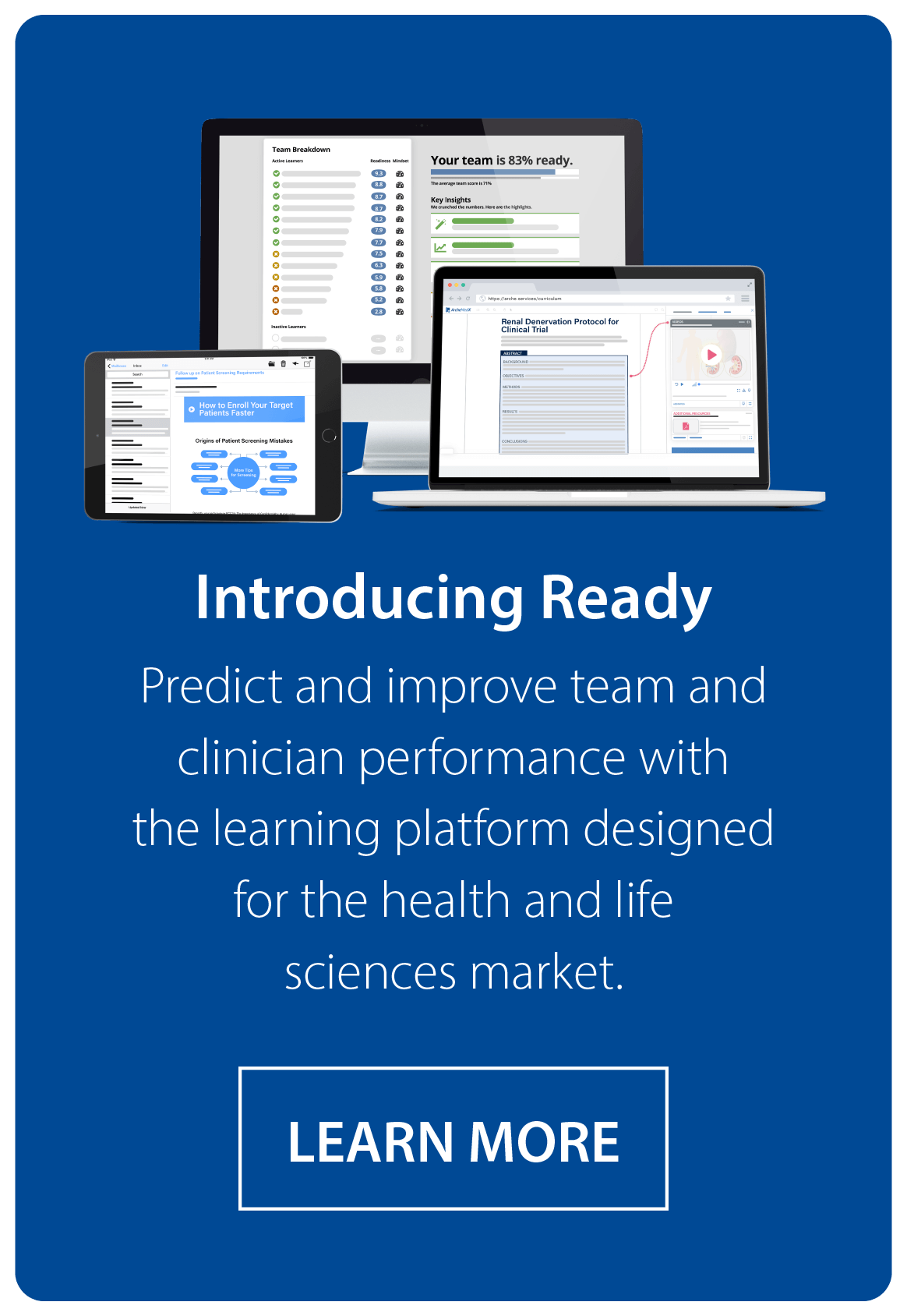
As I described above, using a clinical trial solution like Ready, which is focused on not just training your clinical trial sites, but on predicting their performance, allows you to spot the high performing sites and those with gaps in knowledge or capability.
Better – you can uncover exactly what those gaps are. Then address them before a problem occurs.
Guess less, reduce clinical trial delays.
Sounds nice on paper, but shifting to a more data-centric approach to equipping your trial team requires thought and commitment.
We’ve created a thorough Definitive Guide to Clinical Trial Readiness, which can be a great next step for you as you focus on eliminating clinical trial delays.
Want more help? Take a demo of Ready, and see how you can be accelerating trial timelines with a comprehensive approach to clinical trial readiness.